This study investigated the effects of NMN injected intraperitoneally in mice with sepsis.
Key Points
Important insights into NMN metabolism and efficacy in septic mice were revealed:
- Levels of the NMN Transporter (Slc12a8) were maintained, while levels of NR Transporter (NRK1/2) were diminished
- Levels of NAD+ in the heart and lungs were maintained
- Sepsis-induced inflammation, oxidative stress, and tissue damage were prevented in multiple organs
- NMN was effective, while NR was not in similar septic conditions
- Long-term survival was increased
- Protective effects in cells were dependent on SIRT3
Animal Study Evaluated the Effects of NMN in Sepsis
Sepsis was induced in male mice by feces-injection-in-peritoneum (FIP). Mice serving as control received the same volume of saline.
A single dose of NMN (500 mg/kg body weight) or vehicle was injected intraperitoneally into mice after one hour of FIP (3 g feces per kg body weight). The mice were divided into four groups (n = 15/group):
- Saline + Vehicle: Healthy mice, no treatment
- Saline + NMN: Healthy mice, received NMN
- FIP + Vehicle: Septic mice, no treatment
- FIP + NMN: Septic mice, received NMN
A lower dose of feces (0.8 g feces per kg body weight) was used to evaluate the long-term survival of mice (30 days) with intraperitoneal injection of NMN (100 mg/kg) or vehicle every other day. The mice were divided into two groups (n = 22/group):
- NMN: Septic mice, received NMN
- Vehicle: Septic mice, no treatment
NMN Transporter Levels were Maintained in Septic Mice
NR and NMN are precursors to NAD+, but they can take different paths to get there.
“NR requires NRK1/2 for its conversion to NAD+ within cells, while NMN can enter the cells through its receptor Slc12a8.”
Sepsis affected the levels of enzymes needed for NR conversion, but not NMN.
“Sepsis resulted in significantly lower levels of NRK1/2 mRNA, but not S1c12a8, in the heart, lung, and liver.”
The figures below show the levels of NRK1 (left figure) and NRK2 (right figure) in the lungs were significantly lower in septic mice (Feces, black squares) compared to healthy mice (Saline, white squares).
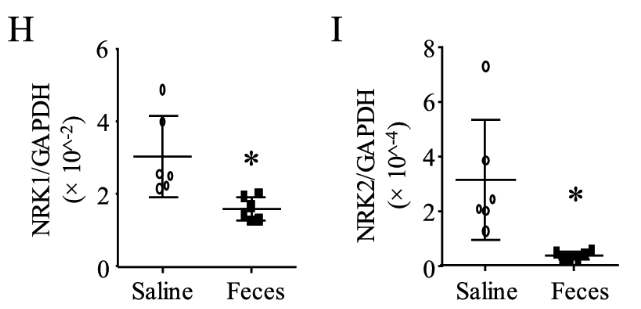
Interestingly, the levels of the NMN transporter, Slc12a8, in the heart, lung, and liver remained unaffected by sepsis.
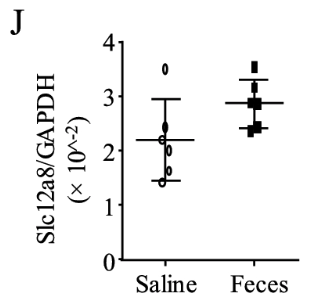
This figure shows the levels of Slc12a8 in the lungs of septic mice (Feces, black squares) were not reduced compared to healthy mice (Saline, white squares).
NMN Prevented Sepsis-Induced NAD+ Depletion
Sepsis caused a dramatic reduction of NAD+ levels in the heart and lungs of untreated mice. However, this was prevented in mice that received NMN.
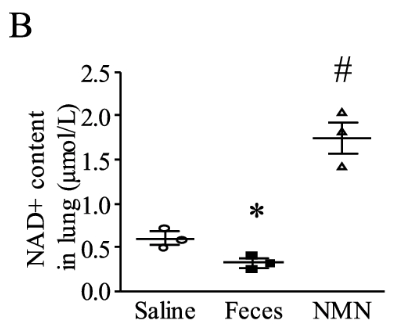
This figure shows the levels of NAD+ in the lungs were significantly reduced in untreated, septic mice (Feces, black squares) compared to healthy mice (Saline, white squares). The lungs of septic mice treated with NMN (NMN, black triangles) showed significantly increased levels of NAD+.
“These results demonstrate that NMN effectively boosts NAD+ levels in sepsis.”
NMN Prevented Sepsis-Induced Organ Injury
Severe health deterioration was evident six hours after sepsis was induced in the mice.
However, analysis of the mice revealed that NMN treatment significantly protected mice from sepsis-induced damage:
- Blood: Prevented elevation in L-Lactate, reduced levels of pro-inflammatory cytokines (TNF-α and IL-1β), and did not affect levels of anti-inflammatory molecules (IL-2 and IL-10)
- Heart: Reduced cell death, infiltration of inflammatory cells, oxidative stress, and preserved heart function
- Lung: Reduced vascular damage, oxidative stress, cell death, inflammatory cell infiltration, and swelling of tiny air sacs called alveoli
- Liver and kidney: Prevented oxidative stress and decreased serum markers of tissue damage
NMN Suggested as Therapy for Sepsis, NR was not
In a previous study, the researchers found NR was only effective in preventing organ damage if given before the onset of sepsis, but not after.
“We found that administration of NR before—but not after—the onset of sepsis prevented organ injury in mice, indicating that the use of NR as a therapeutic approach is limited.”
The current data indicates that the reduced effectiveness of NR after the onset of sepsis is likely due to a decrease in NRK1/2 enzymes associated with sepsis
“This may be due to the reduction of NRK1/2 enzymes during sepsis as the salvage of NAD+ from NR involves NRK1/2 phosphorylating NR.”
The results of this study underscore the critical role of the NMN transporter, Slc12a8, in transporting NMN in septic mice, facilitating a direct increase in NAD+ levels within the cell.
“These results provided a rationale for the use of NMN, but not NR, as a therapy for sepsis.”
NMN Improved Survival of Septic Mice
The effects of NMN (100 mg/kg every other day) on long-term mortality (30 days) were evaluated in septic mice.
“The 30-day mortality was reduced from 36 to 9% by NMN treatment.”
The figure below shows the percentage of mice that survived 30 days after sepsis induction was significantly higher in mice treated with NMN (white triangles) compared to mice that did not receive NMN (black circles).
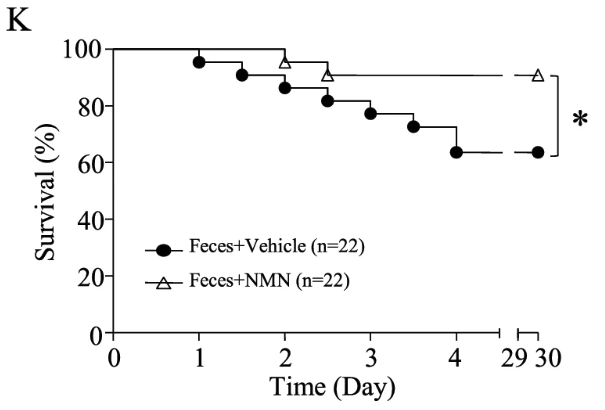
“Our results indicate that treatment with NMN improves survival in sepsis.”
The researchers note the dose of NMN (100 mg/kg) in mice is comparable to 500 mg for humans (60-70 kg body weight), which was well tolerated in a clinical trial.
Sirtuin Signaling Required for Protective Effects of NMN on Septic Damage
Studies in cells revealed how NMN was exerting protective effects on the cells:
- Promoted mitochondrial function
- Enhanced immune cell uptake and degradation of bacteria
- Prevented excessive inflammation and damage
These effects were found to be dependent on the SIRT3 protein, a member of the sirtuin family (“caretaker” proteins essential for cellular health, overall well-being, and longevity).
“NAD+ repletion with NMN prevents mitochondrial dysfunction and restrains bacterial dissemination while limiting inflammatory damage through SIRT3 signaling in sepsis.”
“Thus, NMN may represent a therapeutic option for sepsis.”
Conclusion
Sepsis-associated disruption of the NRK1/2 pathway for NAD+ synthesis emphasized the critical role of NMN transport through the Slc12a8 transporter.
“In contrast to NR, NMN does not require NRK1/2 for its conversion to NAD+.”
Unlike the disrupted NRK1/2 pathway, the Slc12a8 transporter remained unimpeded by sepsis, allowing NMN to effectively elevate NAD+ levels.
NMN prevented sepsis-induced organ damage and improved survival of septic mice.
The protective effects of NMN in the cell were dependent on SIRT3 signaling.
“The present study demonstrates for the first time that therapeutic administration of NMN through NAD+ repletion reduces major organ dysfunction and improves survival in septic mice.”
